DOI: https://doi.org/10.1057/s41599-024-02976-9
تاريخ النشر: 2024-04-15
دور سهولة الاستخدام المدركة، والفائدة، والقوة المالية في اعتماد نظم المعلومات الصحية: الدور الوسيط لحجم المستشفى
الملخص
إن اعتماد نظام معلومات صحية يمثل دائمًا تحديًا للمستشفيات. وذلك لأن معظم الطاقم الطبي لا يمتلك المهارات الكافية لاستخدام التكنولوجيا الجديدة، ولحساسية البيانات الطبية. تشكل هذه العوامل تحديًا لنجاح اعتماد نظام معلومات صحية في المستشفيات. الهدف من هذا البحث هو معرفة العوامل التي تؤثر على اعتماد نظم المعلومات في المستشفيات. وقد بحثت الدراسة في تأثير الوضع المالي للمستشفى؛ وفائدة الاستخدام المدركة وسهولة الاستخدام المدركة على اعتماد نظم المعلومات الصحية من خلال استبيان. تم جمع البيانات من 602 عامل صحي من 20 مستشفى من خلال استبيان مغلق في باكستان، حيث إن اعتماد نظم المعلومات الصحية بطيء جدًا. تم استخدام PLS-SEM للتحليل. تظهر النتائج أن الوضع المالي للمستشفى؛ وفائدة الاستخدام المدركة وسهولة الاستخدام المدركة لها دور إيجابي وذو دلالة في اعتماد نظم المعلومات الصحية. كما تظهر النتائج أن حجم المستشفى يعدل العلاقة بين سهولة الاستخدام المدركة واعتماد نظم المعلومات الصحية، ومن المثير للاهتمام أنه لا يعدل العلاقة بين الفائدة المدركة والقوة المالية تجاه اعتماد نظم المعلومات الصحية. تستنتج الدراسة أن سهولة الاستخدام المدركة، والفائدة المدركة، والقوة المالية هي العوامل الرئيسية اللازمة لاعتماد نظم المعلومات الصحية. تحمل نتائج الدراسة دلالات مفيدة لصانعي السياسات والمهنيين الطبيين لاعتماد نظم المعلومات الصحية بنجاح في المستشفيات. كما توفر أيضًا آفاقًا جديدة للباحثين لاستكشاف عوامل أخرى واختبار هذا الإطار في دول أخرى.
مقدمة
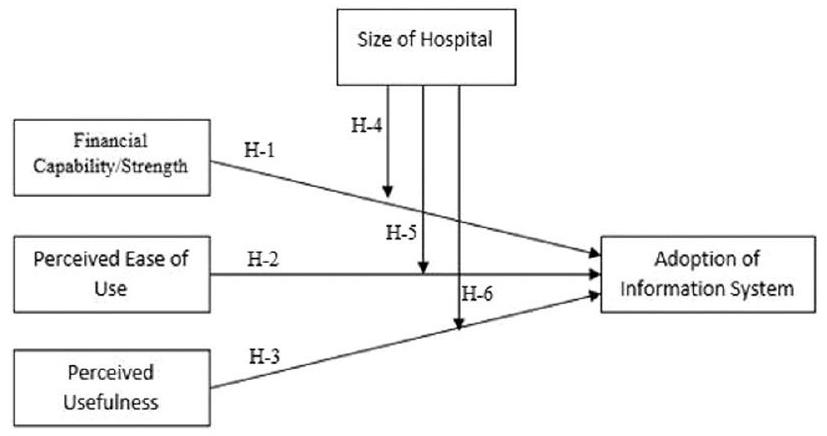
العلاقات بين هذه المتغيرات تهدف إلى اكتشاف الديناميات المعقدة التي تؤثر على اعتماد اتخاذ القرار في نظم المعلومات الصحية. على الرغم من أن هذه العوامل معروفة بأنها مهمة في اعتماد التكنولوجيا، إلا أنه لا يزال هناك فجوة فيما يتعلق بتأثيراتها المشتركة، خاصة عند النظر في أحجام المستشفيات المختلفة (زمان وآخرون 2022). كما أن هناك عملاً محدودًا تم إنجازه حتى الآن حول اعتماد نظم المعلومات الصحية في سياق باكستان. لسد هذه الفجوة، تدرس هذه الدراسة العلاقة بين الفائدة المتوقعة، والسهولة في الاستخدام، والقوة المالية، وتأثير حجم المستشفى كعامل معتدل في اعتماد نظم المعلومات الصحية. على الرغم من أن نظم المعلومات الصحية توفر العديد من الفوائد للمهنيين في الرعاية الصحية وتقديم الخدمات، إلا أن الاعتماد بطيء جدًا في باكستان. ومن الضروري معرفة العوامل التي تعيق هذا الاعتماد. تحتوي الدراسة على الأهداف التالية:
للكشف عن العلاقة بين القوة المالية واعتماد نظام المعلومات الصحية.
(2) لمعرفة العلاقة بين سهولة الاستخدام المدركة واعتماد نظام المعلومات الصحية.
(3) لمعرفة العلاقة بين الفائدة المدركة واعتماد نظم المعلومات الصحية.
(4) لمعرفة الدور الوسيط لحجم المستشفى في العلاقة بين القوة المالية، وفائدة الاستخدام، وتجربة الاستخدام نحو اعتماد نظام المعلومات الصحية.
تكتسب الدراسة أهمية لمطوري التكنولوجيا، والمشرعين، والمهنيين في مجال الرعاية الصحية، خاصة فيما يتعلق بتطوير واعتماد نظم المعلومات الصحية. ستساعد هذه الدراسة صناعة الرعاية الصحية على تطوير استراتيجيات مستنيرة من اعتماد نظم المعلومات الصحية وفقًا لمشهد الرعاية الصحية.
مراجعة الأدبيات
تدريب الموظفين، وتوظيف متخصصي تكنولوجيا المعلومات. لذلك، مقارنةً بالمستشفيات ذات الموارد المالية المنخفضة، فإن تلك التي تتمتع بوضع مالي أفضل تكون أكثر عرضة لاعتماد وتنفيذ نظام المعلومات الصحية بنجاح. العلاقة بين الوضع المالي، وفائدة الاستخدام المدركة، وسهولة الاستخدام المدركة، واعتماد نظام المعلومات الصحية تتأثر بحجم المستشفى. عادةً ما تكون المستشفيات الكبيرة لديها المزيد من الموارد المالية لوضع أنظمة معلومات معقدة واعتماد أنظمة معلومات صحية جديدة. بالإضافة إلى ذلك، قد يكون لديها المزيد من الموظفين والأقسام التي تستخدم النظام، مما يزيد من فائدته المدركة. من ناحية أخرى، قد تجد المستشفيات الصغيرة أنه من الصعب اعتماد نظام المعلومات الصحية، على الرغم من سهولة الاستخدام المدركة وفائدته. تميل هذه المستشفيات أيضًا إلى أن يكون لديها عدد أقل من الموظفين والموارد المالية.
العوامل المتفق عليها لاعتماد التكنولوجيا. المؤشرات المهمة لفائدة الاستخدام المدركة للتكنولوجيا هي؛ تأثيرها على وقت أداء المهام، وتقليل الجهد، وتقليل التكلفة، وفائدتها العامة (السيوف وآخرون 2023؛ ريني وآخرون 2013). إذا كان موظفو منشأة الرعاية الصحية يعتقدون أن نظام المعلومات سيقلل من الوقت المستغرق لأداء مهمة، ويقلل من الجهد، ويقلل من التكلفة، ويكون مفيدًا بشكل عام لهم، فإن موقفهم تجاه الاعتماد سيكون إيجابيًا (أدوتي-ديلوف وآخرون 2023). إذا لم يروا أيًا من العناصر المذكورة أعلاه، فسوف يترددون في اعتماد أنظمة المعلومات. لذلك، يجب على شركات الرعاية الصحية اختيار نظام معلومات يُعتبر مفيدًا وفقًا للمؤشرات المذكورة (ستورمبيرغ وبيرشر 2019).
تتطلب وتحسن الرعاية الصحية (أكتر ونور 2022). يمكن اعتبار نظام المعلومات الصحية الذي يبسط إدارة بيانات المرضى، ويسرع اتخاذ القرارات، ويحسن التواصل بين ممارسي الرعاية الصحية مفيدًا. علاوة على ذلك، فإن سهولة الاستخدام هي عامل رئيسي آخر في اعتماد نظام المعلومات الصحية. تعتبر سهولة استخدام نظام المعلومات الصحية أمرًا حيويًا في الرعاية الصحية حيث يكون الوقت مهمًا جدًا لمهام مختلفة. يساعد التصميم السهل الاستخدام، وسهولة التشغيل جميعها في خلق إحساس جذاب بالفائدة وتشجيع الناس على اعتماد التكنولوجيا (نظامدوست وآخرون 2022).
المنهجية
| عناصر | الفائدة المدركة (هو وأوبراين 2016) |
| 1 | استخدام نظم المعلومات في قطاع الرعاية الصحية يتيح لي العثور على أفضل العروض. |
| 2 | استخدام نظام المعلومات يعزز من فعاليتي في قطاع الرعاية الصحية. |
| ٣ | استخدام نظم المعلومات في قطاع الرعاية الصحية مفيد لي. |
| ٤ | استخدام نظام المعلومات يوفر لي الوقت. |
| سهولة الاستخدام المدركة (بارك 2009) | |
| ٥ | تطبيقات نظم المعلومات الصحية سهلة الاستخدام. |
| ٦ | المرفق الطبي لا يتطلب الكثير من الجهد الذهني إذا تم دعمه بنظام معلومات (تُقدم البدائل من خلال نظام المعلومات). |
| ٧ | المرافق الصحية ليست معقدة للغاية إذا كانت أنظمة المعلومات تقدم لي خدمات. |
| ٨ | من السهل بالنسبة لي تعلم استخدام نظام معلومات الرعاية الصحية المدعوم بالذكاء الاصطناعي. |
| 9 | أن تصبح ماهرًا في استخدام أنظمة المعلومات الصحية أمر سهل. القوة/القدرة المالية (لوك وآخرون 2015) |
| 10 | استخدمت منظمتنا الائتمان بشكل مسؤول. |
| 11 | يمكن لمنظمتي استثمار المال بطريقة صحيحة. |
| 12 | منظمتي تقوم بميزانية الأموال التي لديها بشكل فعال. |
| ١٣ | تنفق منظمتنا أموالها بفعالية على احتياجاتها اليومية. |
| 14 | منظمتي قادرة تمامًا على توفير المال. |
| اعتماد نظام المعلومات (سعيد وعبد النور-هيلم 2008) | |
| 15 | نظام المعلومات يجمع الخدمات التي تقدمها مجالات مختلفة في الجامعة. |
| 16 | تدمج نظم المعلومات بفعالية الخدمات من مجالات مختلفة في الجامعة. |
| 17 | يتيح لي نظام المعلومات الوصول إلى الخدمات من أي مكان داخل الجامعة (تم إسقاطه). |
| ١٨ | يوفر نظام المعلومات بيانات دقيقة. |
| 19 | يوفر نظام المعلومات بيانات منسقة بشكل جيد. |
| 20 | يوفر نظام المعلومات بيانات في الوقت الفعلي (تم إسقاطها) يوفر نظام المعلومات بيانات في الوقت الفعلي (تم إسقاطها). |
| 21 | استخدام نظام المعلومات يعزز من فعاليتي. |
| ٢٢ | استخدام نظام المعلومات يحسن أدائي. |
| 23 | استخدام نظام المعلومات يعزز إنتاجيتي. |
| ٢٤ | بشكل عام، استخدام نظام معلومات مفيد. |
| رقم | نسبة مئوية | |
| جنس | ||
| ذكر | 317 | 52.7% |
| أنثى | ٢٨٥ | ٤٧.٣٪ |
| إجمالي | 602 | 100.0% |
| فئة العمر | ||
| 20-30 سنة | ١٣٠ | 21.2% |
| 31-40 سنة | ٢٦٨ | ٤٣.٧٪ |
| 41-50 سنة | 168 | ٢٧.٤٪ |
| 51 سنة وما فوق | ٣٦ | ٥.٩٪ |
| إجمالي | 602 | 98.2% |
| تعيين | ||
| طبيب | ٣١٥ | 52.3٪ |
| مُرَاعِيَة | 287 | ٤٧.٧٪ |
| إجمالي | 602 | 100.0% |
تشير الجدول إلى توزيعهم حسب العمر، مما يدل على أن 130 كانوا في الفئة العمرية من
النتائج والاكتشافات
| الجدول 3: الموثوقية، التعددية الخطية، والصلاحية التوافقية. | ||||||
| بناء | عناصر | الأحمال الخارجية | VIF | كاليفورنيا | سي آر | AVE |
| تكييف نظام المعلومات | AIS2 | 0.673 | 1.740 | 0.874 | 0.900 | 0.532 |
| AIS3 | 0.644 | 1.505 | ||||
| AIS4 | 0.735 | 1.993 | ||||
| AIS5 | 0.774 | 2.063 | ||||
| AIS6 | 0.713 | 1.895 | ||||
| AIS7 | 0.779 | 2.012 | ||||
| AIS8 | 0.703 | 1.748 | ||||
| AIS10 | 0.801 | 1.977 | ||||
| القدرة المالية | FSC1 | 0.747 | 1.885 | 0.883 | 0.914 | 0.680 |
| FSC2 | 0.848 | ٢.٢١٤ | ||||
| FSC3 | 0.834 | ٢.٥٢٣ | ||||
| FSC4 | 0.886 | 2.921 | ||||
| FSC7 | 0.800 | 1.787 | ||||
| سهولة الاستخدام المدركة | PEU2 | 0.697 | 1.445 | 0.649 | 0.794 | 0.565 |
| PEU3 | 0.712 | 1.345 | ||||
| PEU4 | 0.838 | 1.175 | ||||
| الفائدة المدركة | PUF1 | 0.805 | 2.295 | 0.882 | 0.907 | 0.583 |
| PUF2 | 0.781 | 2.206 | ||||
| PUF3 | 0.793 | 2.332 | ||||
| PUF4 | 0.٦٩٩ | 1.885 | ||||
| PUF6 | 0.772 | ٢.٢٤٩ | ||||
| PUF7 | 0.734 | 1.704 | ||||
| PUF8 | 0.758 | 1.978 | ||||
| حجم المستشفى | SOH1 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| تكييف نظام المعلومات | القدرة المالية | سهولة الاستخدام المدركة | الفائدة المدركة | حجم المستشفى | |
| تكييف نظام المعلومات | 0.729 | ||||
| القدرة المالية | 0.274 | 0.825 | |||
| سهولة الاستخدام المدركة | 0.167 | 0.303 | 0.751 | ||
| الفائدة المدركة | 0.315 | 0.737 | 0.312 | 0.764 | |
| حجم المستشفى | -0.015 | 0.121 | 0.09 | 0.143 | 1.000 |
| تكييف نظام المعلومات | القدرة المالية | سهولة الاستخدام المدركة | الفائدة المدركة | |
| القدرة المالية | 0.292 | |||
| سهولة الاستخدام المدركة | 0.215 | 0.366 | ||
| الفائدة المدركة | 0.34 | 0.837 | 0.389 | |
| حجم المستشفى | 0.065 | 0.131 | 0.095 | 0.16 |
| فرضية |
|
إحصائيات T |
|
النتائج |
| H1: FC -> AIS | 0.168 | 1.995 | 0.023 | مدعوم |
| H2: بي إي يو -> إيه آي إس | 0.076 | 1.981 | 0.044 | مدعوم |
| H3: PU -> AIS | 0.254 | ٤.١٦٢ | 0.000 | مدعوم |
| H4: FC/SOH/AIS > AIS | -0.075 | 1.246 | 0.213 | غير مدعوم |
| H5: PEU/SOH/AIS > AIS | 0.101 | ٢.٦١٨ | 0.009 | مدعوم |
| H6: PUS/SOH/AIS > AIS | 0.08 | 1.073 | 0.283 | غير مدعوم |
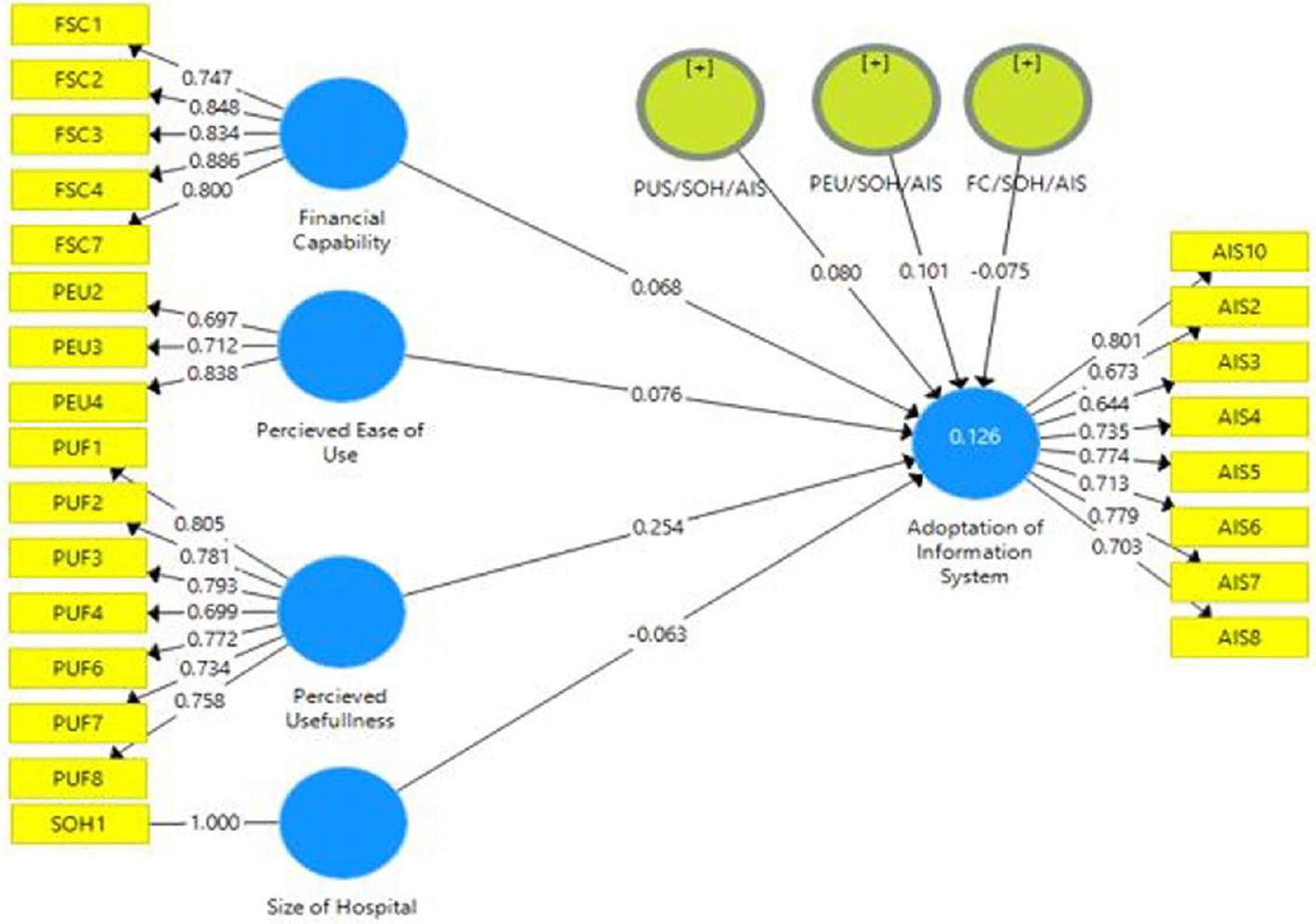
تظهر قيم تحليل الانحدار أن هناك علاقة إيجابية وذات دلالة بين FC واعتماد نظام المعلومات الصحية
تظهر قيم تحليل الانحدار أن هناك علاقة إيجابية وذات دلالة بين PEU واعتماد HIS مع
الدور المهم لتصور سهولة الاستخدام في اعتماد نظم المعلومات الصحية إيجابي وذو دلالة. بعبارة أخرى، يؤثر تصور سهولة الاستخدام بشكل إيجابي على اعتماد نظم المعلومات الصحية.
تظهر قيم تحليل الانحدار أن هناك علاقة إيجابية وذات دلالة بين استخدام التكنولوجيا (PU) واعتماد نظام المعلومات الصحية (HIS) مع
| نموذج مشبع | النموذج المقدر | |
| SRMR | 0.068 | 0.068 |
| d_ULS | 1.391 | 1.391 |
| d_G | 0.524 | 0.524 |
| مربع كاي | ١٧٩٦.٥٢٢ | ١٧٩٦.٥٢٢ |
| NFI | 0.76 | 0.76 |
| تسجيل الدخول الموحد | SSE |
|
|
معامل التحديد (R مربع) | |
| نظام المعلومات الآلي | ٤٨١٦ | ٤٥٦٣.٦٧٣ | 0.052 | 0.126 | 0.000 |
| FC | ٣٠١٠ | ٣٠١٠ | |||
| بيو | 1806 | 1806 | |||
| PU | 4214 | 4214 | |||
| سو | 602 | 602 |
| تكييف نظام المعلومات | أهمية | العروض |
| القدرة المالية | 0.078 | 62.56 |
| بيو | 0.101 | ٥٩.٠٢٢ |
| PU | 0.365 | 68.297 |
| العلاقات |
|
|
| H1: FC -> AIS | -0.027 | 0.827 |
| H2: بي إي يو -> إيه آي إس | 0.031 | 0.683 |
| H3: PU -> AIS | -0.157 | 0.190 |
| H4: FC/SOH/AIS -> AIS | 0.095 | 0.464 |
| H5: PEU/SOH/AIS -> AIS | -0.006 | 0.940 |
| H6: PUS/SOH/AIS -> AIS | 0.073 | 0.610 |
| العلاقات |
|
|
| H1: FC -> AIS | 0.120 | 0.312 |
| H2: بي إي يو -> إيه آي إس | 0.006 | 0.899 |
| H3: PU -> AIS | -0.270 | 0.027 |
| H4: FC/SOH/AIS -> AIS | 0.006 | 0.981 |
| H5: PEU/SOH/AIS -> AIS | 0.014 | 0.854 |
| H6: PUS/SOH/AIS -> AIS | -0.041 | 0.772 |
مسؤول عن تكييف نظام المعلومات (Chen et al. 2020). تم تقديم ست فرضيات استنادًا إلى نموذج هذه الدراسة، من بينها ثلاث فرضيات تستند إلى علاقات مباشرة، والأخرى تستند إلى علاقات معتدلة. من بين هذه الست، لم تدعم النتائج سوى فرضيتين، بينما تم دعم الأربع الأخرى. تدعي الفرضية الأولى أن القدرة المالية ستؤدي إلى تحسين تكييف نظام المعلومات في قطاع الرعاية الصحية في باكستان. ومع ذلك، تدعم نتائج هذه الدراسة الفرضية المدعاة مع
طبيعة البيانات الحساسة، التي تحتاج إلى اعتماد تقنيات مفيدة وسهلة الاستخدام (Huarng et al. 2022). وبالمثل، فإن القدرة المالية (Endriyas et al. 2023) لمنظمة الرعاية الصحية أيضًا حاسمة حيث يتطلب اعتماد نظم المعلومات الصحية استثمارات كبيرة في المرافق التكنولوجية، والتدريب، والصيانة. قد تواجه المستشفيات صعوبات في اعتماد ودمج نظم المعلومات الصحية إذا كانت تعاني من صعوبات مالية. قد يعيق ذلك قدرتها على الاستفادة الكاملة من نظم المعلومات الصحية لتقديم خدمات أفضل. لذلك، فإن اعتبار PEU و PU والقدرة المالية هي عوامل حاسمة لاستراتيجيات اعتماد نظم المعلومات الصحية. بالإضافة إلى ذلك، بحثت الدراسة أيضًا في التأثير المعدل لحجم المستشفى (Kraus et al. 2021) على تأثير PU و PEU والقدرة المالية على اعتماد نظم المعلومات الصحية. من الواضح من النتائج أن حجم المستشفى له دور معدل على تأثير PEU على اعتماد نظم المعلومات الصحية. بعبارة أخرى، يعتمد دور PEU على اعتماد نظم المعلومات الصحية على حجم المستشفى. قد يؤثر PEU على اعتماد نظم المعلومات الصحية في المستشفيات الكبيرة أكثر من المستشفيات الصغيرة، حيث أن المستشفيات الكبيرة لديها موارد تنظيمية وتعقيدات أكثر من الصغيرة. نظرًا لأهمية هذا التأثير المعدل، يجب تكييف تدابير تعزيز PEU وفقًا للاحتياجات المحددة المرتبطة بأحجام المستشفيات. من الضروري فهم العلاقة بين حجم المستشفى و PEU في التأثير على اعتماد نظم المعلومات الصحية من أجل وضع استراتيجيات وتدابير مخصصة وفقًا للاحتياجات والصعوبات المختلفة التي تواجهها منظمات الرعاية الصحية ذات الأحجام المختلفة. كما أظهرت النتائج، لا يوجد دور معدل كبير لحجم المستشفى على العلاقة بين القدرة المالية و PU واعتماد نظم المعلومات الصحية. تأثير القدرة المالية و PU على اعتماد نظم المعلومات الصحية مشابه في المستشفيات ذات الأحجام المختلفة. بعبارة أخرى، فإن PU والقدرة التمويلية لهما تأثير كبير على قرار اعتماد نظم المعلومات الصحية، بغض النظر عن حجم المستشفى. غياب هذا التأثير المعدل يشير إلى أن التكتيكات لزيادة PU وتوفير التمويل لاعتماد نظم المعلومات الصحية يجب أن تُستخدم على نطاق واسع في جميع المستشفيات من جميع الأحجام. ويؤكد على أهمية هذه العناصر كعوامل قابلة للتطبيق على نطاق واسع لاعتماد نظم المعلومات الصحية عبر جميع المستشفيات. تحتوي الدراسة على الآثار التالية.
الخاتمة
التوصيات.
- يجب على منظمات الصحة تخصيص أموال لاعتماد التكنولوجيا الجديدة (Poon et al. 2004).
- لنجاح تنفيذ أو اعتماد نظام معلومات، يجب على الشركات اختيار النظام الذي يُعتبر مفيدًا وسهلاً (Nezamdoust et al. 2022; Zaman et al. 2022).
- يجب على المستشفيات، وما إلى ذلك، تدريب موظفيها على فائدة النظام الجديد قبل التنفيذ (Pedota et al. 2023).
- تحتاج المستشفيات الكبيرة إلى اختيار أكثر دقة لنظم المعلومات الصحية حيث ستشارك العديد من الأطراف في الاستخدام (Yusif et al. 2022).
القيود والأعمال المستقبلية.
- يمكن دمج نظريات و متغيرات أخرى في الإطار في المستقبل لجعله أكثر شمولاً.
- نظرًا لأن هذه الدراسة أجريت في باكستان، يمكن أيضًا اختبار الإطار في دول أخرى لاختبار قابليته للتعميم.
- هناك حاجة إلى مزيد من البحث لاستكشاف تأثير حجم المستشفى على العلاقة بين قرحة الضغط والقوة المالية.
توفر البيانات
نُشر على الإنترنت: 15 أبريل 2024
References
Ahmad SF, Alam MM, Rahmat MK, Mubarik MS, Hyder SI (2022) Academic and administrative role of artificial intelligence in education. Sustainability 14(3):1101. https://doi.org/10.3390/su14031101
Ahmad SF, Rahmat MK, Mubarik MS, Alam MM, Hyder SI (2021) Artificial intelligence and its role in education. Sustainability 13(22):12902. https://doi. org/10.3390/su132212902
Akther T, Nur T (2022) A model of factors influencing COVID-19 vaccine acceptance: a synthesis of the theory of reasoned action, conspiracy theory belief, awareness, perceived usefulness, and perceived ease of use. PLoS ONE 17(1):e0261869. https://doi.org/10.1371/journal.pone. 0261869
Alboliteeh M, Alrashidi MS, Alrashedi N, Gonzales A, Mostoles RJ, Pasay-an E, Dator WL (2022) Knowledge management and sustainability performance of hospital organisations: the healthcare managers’ perspective. Sustainability 15(1):203. https://doi.org/10.3390/su15010203
Almaiah MA, Alhumaid K, Aldhuhoori A, Alnazzawi N, Aburayya A, Alfaisal R, Salloum SA, Lutfi A, Al Mulhem A, Alkhdour T, Awad AB, Shehab R (2022) Factors affecting the adoption of digital information technologies in higher education: an empirical study. Electronics 11(21):3572. https://doi.org/10. 3390/electronics11213572
Alotaibi Y, Subahi AF (2022) New goal-oriented requirements extraction framework for e-health services: a case study of diagnostic testing during the COVID-19 outbreak. Bus Process Manag J 28(1):273-292. https://doi.org/10. 1108/BPMJ-09-2020-0414
Alsyouf A, Lutfi A, Alsubahi N, Alhazmi FN, Al-Mugheed K, Anshasi RJ, Alharbi NI, Albugami M (2023) The use of a technology acceptance model (TAM) to predict patients’ usage of a personal health record system: the role of security, privacy, and usability. Int J Environ Res Public Health 20(2):1347. https://doi. org/10.3390/ijerph20021347
Barney J (1991) Firm resources and sustained competitive advantage. J Manag 17(1):99-120. https://doi.org/10.1177/014920639101700108
Bloomberg J (2018) Digitization, digitalization, and digital transformation: confuse them at your peril. Forbes
Broccardo L, Zicari A, Jabeen F, Bhatti ZA (2023) How digitalization supports a sustainable business model: a literature review. Technol Forecast Soc Change 187:122146. https://doi.org/10.1016/j.techfore.2022.122146
Brown SA, Dennis AR, Venkatesh V (2010) Predicting collaboration technology use: integrating technology adoption and collaboration research. J Manag Inf Syst 27(2):9-54. https://doi.org/10.2753/MIS0742-1222270201
Chen L, Aklikokou AK (2020) Determinants of E-government adoption: testing the mediating effects of perceived usefulness and perceived ease of use. Int J Public Adm 43(10):850-865. https://doi.org/10.1080/01900692.2019.1660989
Chen P-T, Lin C-L, Wu W-N (2020) Big data management in healthcare: adoption challenges and implications. Int J Inf Manag 53:102078. https://doi.org/10. 1016/j.ijinfomgt.2020.102078
Cheng N, Li H, Bang Y (2023) Pay-for-performance schemes and hospital HIT adoption. Decis Support Syst 164:113868. https://doi.org/10.1016/j.dss.2022. 113868
Crisan EL, Mihaila A (2023) Health-care information systems adoption-a review of management practices. Vilakshan XIMB J Manag 20(1):130-139. https:// doi.org/10.1108/XJM-04-2021-0121
Dewar RD, Dutton JE (1986) The adoption of radical and incremental innovations: an empirical analysis. Manag Sci 32(11):1422-1433
Davis FD (1989) Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q 13(3):319. https://doi.org/10.2307/249008
Deepu TS, Ravi V (2021) Supply chain digitalization: an integrated MCDM approach for inter-organizational information systems selection in an electronic supply chain. Int J Inf Manag Data Insights 1(2):100038. https://doi. org/10.1016/j.jjimei.2021.100038
Dhagarra D, Goswami M, Kumar G (2020) Impact of trust and privacy concerns on technology acceptance in healthcare: an Indian perspective. Int J Med Inform 141:104164. https://doi.org/10.1016/j.ijmedinf.2020.104164
Dicuonzo G, Donofrio F, Fusco A, Shini M (2023) Healthcare system: moving forward with artificial intelligence. Technovation 120:102510. https://doi.org/ 10.1016/j.technovation.2022.102510
Hedayati MK, Schniederjans DG (2022) Integration of knowledge management in digital healthcare industries. In: Wang J (ed) Encyclopedia of data science and machine learning. IGI Global United States of America, p 1703-1716. https:// doi.org/10.4018/978-1-7998-9220-5.ch102
Hopper AM (2015) Using data management techniques to modernize healthcare. Productivity Press
Huarng K-H, Yu TH-K, Lee CF (2022) Adoption model of healthcare wearable devices. Technol Forecast Soc Change 174:121286. https://doi.org/10.1016/j. techfore.2021.121286
Ibrahim M, Shahid MK, Ahmed SF (2014) The impact of telecom services characteristics on consumer for use in Pakistan. Adv Econ Bus 2(4):172-179. https://doi.org/10.13189/aeb.2014.020403
Ibrahim M, Shahid M, Akbar S, Ahmed SF (2015) Determining the effect of innovations for mobile banking adoption in Pakistan. J Inf Eng Appl 5(11):16-23
Jarva E, Oikarinen A, Andersson J, Tomietto M, Kääriäinen M, Mikkonen K (2023) Healthcare professionals’ digital health competence and its core factors; development and psychometric testing of two instruments. Int J Med Inform 171:104995. https://doi.org/10.1016/j.ijmedinf.2023.104995
Khan Y, Su’ud MBM, Alam MM, Ahmad SF, Ahmad (Ayassrah) AYAB, Khan N (2022a) Application of internet of things (IoT) in sustainable supply chain management. Sustainability 15(1):694. https://doi.org/10.3390/su15010694
Khan Y, Su’ud MBM, Alam MM, Ahmad SF, Salim NA, Khan N (2022b) Architectural threats to security and privacy: a challenge for internet of things (IoT) applications. Electronics 12(1):88. https://doi.org/10.3390/electronics12010088
Khanna RR, Murray SG, Wen T, Salmeen K, Illangasekare T, Benfield N, AdlerMilstein J, Savage L (2022) Protecting reproductive health information in the post-Roe era: interoperability strategies for healthcare institutions. J Am Med Inform Assoc 30(1):161-166. https://doi.org/10.1093/jamia/ocac194
Kim D-Y, Jang S (Shawn), Morrison AM (2011) Factors affecting organizational information technology acceptance: a comparison of convention and visitor bureaus and meeting planners in the United States. J Conv Event Touri 12(1):1-24. https://doi.org/10.1080/15470148.2010.551291
Kraus S, Schiavone F, Pluzhnikova A, Invernizzi AC (2021) Digital transformation in healthcare: analyzing the current state-of-research. J Bus Res 123:557-567. https://doi.org/10.1016/j.jbusres.2020.10.030
Kuan KKY, Chau PYK (2001) A perception-based model for EDI adoption in small businesses using a technology-organization-environment framework. Inf Manag 38(8):507-521. https://doi.org/10.1016/S0378-7206(01)00073-8
Kuek A, Hakkennes S (2020) Healthcare staff digital literacy levels and their attitudes towards information systems. Health Inform J 26(1):592-612. https:// doi.org/10.1177/1460458219839613
LaBerge L (2020) How COVID-19 has pushed companies over the technology tipping point-and transformed business forever. Mckinsey. https://www. mckinsey.com/capabilities/strategy-and-corporate-finance/our-insights/how-covid-19-has-pushed-companies-over-the-technology-tipping-point-and-transformed-business-forever
Lee G, Xia W (2006) Organizational size and IT innovation adoption: a metaanalysis. Inf Manag 43(8):975-985. https://doi.org/10.1016/j.im.2006.09.003
Lin C, Lin I-C, Roan J (2012) Barriers to physicians’ adoption of healthcare information technology: an empirical study on multiple hospitals. J Med Syst 36(3):1965-1977. https://doi.org/10.1007/s10916-011-9656-7
Liu X, Ahmad SF, Anser MK, Ke J, Irshad M, Ul-Haq J, Abbas S (2022) Cyber security threats: a never-ending challenge for e-commerce. Front Psychol 13. https://doi.org/10.3389/fpsyg.2022.927398
Lind MR, Zmud RW, Fischer WA (1989) Microcomputer adoption-the impact of organizational size and structure. Inf Manag 16(3):157-162
Loke V, Choi L, Libby M (2015) Increasing Youth Financial Capability: An Evaluation of the MyPath Savings Initiative. J Consum Aff 49(1):97-126. https:// doi.org/10.1111/joca. 12066
Mahdi SS, Battineni G, Khawaja M, Allana R, Siddiqui MK, Agha D (2023) How does artificial intelligence impact digital healthcare initiatives? A review of AI applications in dental healthcare. Int J Inf Manag Data Insights 3(1):100144. https://doi.org/10.1016/j.jjimei.2022.100144
Malik M, Kazi AF, Hussain A (2021) Adoption of health technologies for effective health information system: need of the hour for Pakistan. PLoS ONE 16(10):e0258081. https://doi.org/10.1371/journal.pone. 0258081
McAdory BJ (2021) Investment in information technology can improve profitability in U.S. hospitals. https://harbert.auburn.edu/news/investment-in-information-technology-can-improve-profitability-in-us-hospitals.html
Mousa S, Bouraoui T (2023) The role of sustainability and innovation in financial services business transformation. Theor Econ Lett 13(1):84-108. https://doi. org/10.4236/tel.2023.131005
Ndayishimiye C, Lopes H, Middleton J (2023) A systematic scoping review of digital health technologies during COVID-19: a new normal in primary health care delivery. Health Technol. https://doi.org/10.1007/s12553-023-00725-7
Nezamdoust S, Abdekhoda M, Rahmani A (2022) Determinant factors in adopting mobile health application in healthcare by nurses. BMC Med Inform Decis Mak 22(1):47. https://doi.org/10.1186/s12911-022-01784-y
Nikou S, Maslov I (2021) An analysis of students’ perspectives on e-learning participation-the case of COVID-19 pandemic. Int J Inf Learn Technol 38(3):299-315. https://doi.org/10.1108/IJILT-12-2020-0220
Park DY, Kim H (2023) Determinants of intentions to use digital mental healthcare content among university students, faculty, and staff: motivation, perceived usefulness, perceived ease of use, and parasocial interaction with AI Chatbot. Sustainability 15(1):872. https://doi.org/10.3390/su15010872
Park SY (2009) An Analysis of the Technology Acceptance Model in Understanding University Students’ Behavioral Intention to Use e-Learning. Edu Technol Soc 12(3):150-162
Pedota M, Grilli L, Piscitello L (2023) Technology adoption and upskilling in the wake of Industry 4.0. Technol Forecast Soc Change 187:122085. https://doi. org/10.1016/j.techfore.2022.122085
Philibert C (2003) Technology innovation, development and diffusion. https:// www.oecd.org/env/cc/2956490.pdf
Poon EG, Blumenthal D, Jaggi T, Honour MM, Bates DW, Kaushal R (2004) Overcoming barriers to adopting and implementing computerized physician order entry systems in U.S. hospitals. Health Aff 23(4):184-190. https://doi. org/10.1377/hlthaff.23.4.184
Prasad A (2018) 10 ways technology has reshaped the modern workplace. Quickfms. https://www.quickfms.com/blog/how-technology-has-reshaped-the-workplace
Pufahl L, Zerbato F, Weber B, Weber I (2022) BPMN in healthcare: challenges and best practices. Inf Syst 107:102013. https://doi.org/10.1016/j.is.2022.102013
Renny, Guritno S, Siringoringo H (2013) Perceived usefulness, ease of use, and attitude towards online shopping usefulness towards online airlines ticket purchase. Procedia Soc Behav Sci 81:212-216. https://doi.org/10.1016/j. sbspro.2013.06.415
Rey-Moreno M, Periáñez-Cristóbal R, Calvo-Mora A (2022) Reflections on sustainable urban mobility, mobility as a service (MaaS) and adoption models. Int J Environ Res Public Health 20(1):274. https://doi.org/10.3390/ ijerph20010274
Rohani N, Yusof MM (2023) Unintended consequences of pharmacy information systems: a case study. Int J Med Inform 170:104958. https://doi.org/10.1016/j. ijmedinf.2022.104958
Saeed KA, Abdinnour-Helm S (2008) Examining the effects of information system characteristics and perceived usefulness on post adoption usage of information systems. Inf Manag 45(6):376-386. https://doi.org/10.1016/j. im.2008.06.002
Salah OH, Yusof ZM, Mohamed H (2021) The determinant factors for the adoption of CRM in the Palestinian SMEs: the moderating effect of firm size. PLoS ONE 16(3):e0243355. https://doi.org/10.1371/journal.pone. 0243355
Sayed AF, Shahid MK, Ahmad SF (2020) Adoption of mobile payment application and its impact on business. pp. 253-269. https://doi.org/10.4018/978-1-7998-2398-8.ch012
Shahadat MMH, Nekmahmud M, Ebrahimi P, Fekete-Farkas M (2023) Digital technology adoption in SMEs: what technological, environmental and organizational factors influence in emerging countries? Glob Bus Rev 097215092211371. https://doi.org/10.1177/09721509221137199
Shahzad K, Jianqiu Z, Zia MA, Shaheen A, Sardar T (2021) Essential factors for adopting hospital information system: a case study from Pakistan. Int J Comput Appl 43(1):26-37. https://doi.org/10.1080/1206212X.2018.1504460
Singerman A, Lence SH (2023) The source of uncertainty influences technology adoption. Eur Rev Agric Econ. https://doi.org/10.1093/erae/jbac036
Sinhasane S (2022) What is health information system and its significance in the healthcare sector? https://mobisoftinfotech.com/resources/blog/importance-of-health-information-system/
Stachwitz P, Debatin JF (2023) Digitalisierung im Gesundheitswesen: heute und in Zukunft. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 66(2):105-113. https://doi.org/10.1007/s00103-022-03642-8
Sturmberg JP, Bircher J (2019) Better and fulfilling healthcare at lower costs: the need to manage health systems as complex adaptive systems. F1000Research 8:789. https://doi.org/10.12688/f1000research.19414.1
Tortorella GL, Fogliatto FS, Espôsto KF, Mac Cawley Vergara A, Vassolo R, Tlapa Mendoza D, Narayanamurthy G (2022) Measuring the effect of Healthcare 4.0 implementation on hospitals’ performance. Prod Plan Control 33(4):386-401. https://doi.org/10.1080/09537287.2020.1824283
Tsai M-F, Hung S-Y, Yu W-J, Chen CC, Yen DC (2019) Understanding physicians’ adoption of electronic medical records: healthcare technology self-efficacy, service level and risk perspectives. Comput Stand Interfaces 66:103342. https://doi.org/10.1016/j.csi.2019.04.001
Tseng M-L, Ha HM, Wu K-J, Xue B (2022) Healthcare industry circular supply chain collaboration in Vietnam: vision and learning influences on connection in a circular supply chain and circularity business model. Int J Logist Res Appl 25(4-5):743-768. https://doi.org/10.1080/13675567.2021.1923671
Vassolo RS, Mac Cawley AF, Tortorella GL, Fogliatto FS, Tlapa D, Narayanamurthy G (2021) Hospital investment decisions in healthcare 4.0 technologies: scoping review and framework for exploring challenges, trends, and research directions. J Med Internet Res 23(8):e27571. https://doi.org/10. 2196/27571
Veikkolainen P, Tuovinen T, Jarva E, Tuomikoski A-M, Männistö M, Pääkkönen J, Pihlajasalo T, Reponen J (2023) eHealth competence building for future doctors and nurses-attitudes and capabilities. Int J Med Inform 169:104912. https://doi.org/10.1016/j.ijmedinf.2022.104912
Venkatesh V, Thong JYL, Xu X (2012) Consumer acceptance and use of information technology: extending the unified theory of acceptance and use of technology. MIS Q 36(1):157. https://doi.org/10.2307/41410412
Wang BB, Wan TTH, Burke DE, Bazzoli GJ, Lin BYJ (2005) Factors influencing health information system adoption in American hospitals. Health Care Manag Rev 30(1):44-51
Xiong E (2021) The sustainable impact of a paperless office. Forbes. https://www. forbes.com/sites/forbestechcouncil/2021/05/11/the-sustainable-impact-of-a-paperless-office/?sh=1fb81b421095
Yulianto A, Ahmad S, Lelly A, Nobia S (2022) Ease of use technology as a dominant factor in technology acceptance hospital information system by officers at the Jambi provincial government hospital. In: Proceedings of the 5th European international conference on industrial engineering and operations management Rome, Italy, July 26-28, 2022. IEOM Society International
Yusif S, Hafeez-Baig A, Soar J (2022) Change management and adoption of health information technology (HIT)/eHealth in public hospitals in Ghana: a qualitative study. Appl Comput Inform 18(3/4):279-289. https://doi.org/10.1016/ j.aci.2019.11.007
Zhao Y, Li K, Zhang L (2019) A meta-analysis of online health adoption and the moderating effect of economic development level. Int J Med Inform 127:68-79. https://doi.org/10.1016/j.ijmedinf.2019.04.015
شكر وتقدير
مساهمات المؤلفين
المصالح المتنافسة
الموافقة الأخلاقية
الموافقة المستنيرة
معلومات إضافية
ملاحظة الناشر: تظل شركة سبرينغر ناتشر محايدة فيما يتعلق بالمطالبات القضائية في الخرائط المنشورة والانتماءات المؤسسية.
© المؤلف(ون) 2024
كلية الاقتصاد والإدارة، جامعة شنغهاي بوليتكنيك، شنغهاي 201209، الصين. معهد إدارة الأعمال، كراتشي، باكستان. كلية إدارة الأعمال، جامعة الملك سعود، الرياض، المملكة العربية السعودية. المعهد الدولي للدراسات الاجتماعية (ISS)، جامعة إيراسموس روتردام، كورتيناركاد 12، 2518 AX لاهاي، هولندا. قسم علوم الإدارة، جامعة غوايدر، غوايدر، باكستان. البريد الإلكتروني:فايز.أحمد@iobm.edu.pk; ou@iss.nl
DOI: https://doi.org/10.1057/s41599-024-02976-9
Publication Date: 2024-04-15
Role of perceived ease of use, usefulness, and financial strength on the adoption of health information systems: the moderating role of hospital size
Abstract
Adoption of a health information system is always a challenge for hospitals. It is because most of the medical staff do not have enough skills to use the new technology and due to the sensitivity of medical data. These factors pose a challenge for the successful adoption of health information system in hospitals. The aim of this research is to find out the factors which influence the adoption of information systems in hospitals. The study investigated the impact of the Financial status of the Hospital; Perceived Usefulness and Perceived Ease of Use on the adoption of health information systems through a questionnaire survey. Data was collected from 602 healthcare workers from 20 hospitals through close-ended questionnaire in Pakistan, where the adoption of health information systems is very slow. PLS-SEM was used for the analysis. The findings show that the Financial status of the Hospital; Perceived Usefulness and Perceived Ease of Use have positive and significant role in the adoption of Health Information Systems. The finding also shows that hospital size moderates the relationship of Perceived ease of use and the adoption of health information systems and interestingly it does not moderate the relationship among perceived usefulness and financial strength toward the adoption of health information systems. The study concludes that perceived ease of use, perceived usefulness and financial strength are the main factors, necessary for the adoption of health information systems. The findings of the study have useful implications for policy makers, medical professionals to successfully adopt health information systems in hospitals. It also provides new avenues for researchers to explore other factors and test this framework in other countries.
Introduction
relationships among these variables is to find out the complex dynamics that influence the adoption of HIS decision-making. Although these factors are known to be important in the adoption of technology, there still exists a gap regarding their combined effects, especially when considering different hospital sizes (Zaman et al. 2022). There is also limited work done so far on HIS adoption in the context of Pakistan. To fill the gap, this study examines the relationship between PU, PEU, financial strength and the moderating impact of hospital size in the adoption of HIS. Despite the fact that HIS provides many benefits for healthcare professionals and delivery, the adoption is too slow in Pakistan. And it is necessary to find out the factors which hinders this adoption. The study has the following objectives:
(1) To find out the relationship between financial strength and HIS adoption.
(2) To find out the relationship between perceived ease of use and HIS adoption.
(3) To find out the relationship between perceived usefulness and HIS adoption.
(4) To find out the moderating role of hospital size on the relationship between financial strength, PU and PEU toward the adoption of HIS.
The study has significance for technology developers, legislators, and healthcare professionals especially for the development, and adoption of HIS. It will facilitate the healthcare industry to develop well-informed strategies from HIS adoption according to the healthcare landscape.
Literature review
training employees, and recruiting IT specialists. Therefore, compared to hospitals with low financial resources, those with better financial standing are more likely to adopt and implement a HIS successfully. The association between financial situation, perceived usefulness, perceived ease of use, and HIS adoption is moderated by the hospital size. Larger hospitals typically have more financial resources and to put complex ISs in place and adopt new HIS. Additionally, they could have more staff and divisions that use the system, increasing its perceived usefulness. Smaller hospitals, on the other hand, may find it more difficult to adopt an HIS, despite their perceived ease of use and usefulness. These hospitals also tend to have fewer staff members and financial resources.
agreed-upon factors for technology adoption. The important indicators for PU of technology are; its influence on task performance time, effort reduction, cost reduction, and general usefulness (Alsyouf et al. 2023; Renny et al. 2013). If the employees of a healthcare facility believe that the IS will reduce the time it takes to perform a task, reduce effort, reduce cost, and be generally useful for them, their attitude toward the adoption will be positive (Addotey-Delove et al. 2023). If they do not see any of the above elements, then they will be reluctant to adopt IS. Therefore, healthcare firms must choose an IS that is perceived to be useful according to the mentioned indicators (Sturmberg and Bircher 2019).
requirements and improves healthcare (Akther and Nur 2022). A HIS that simplifies the management of patient data, expedites decision-making, and improves communication between healthcare practitioners could be considered useful. Furthermore, PEU is another key factor for HIS adoption. The PEU of the HIS is crucial in healthcare where time is very important for various tasks. A user-friendly design, and easy operation all help to create an appealing sense of usefulness and encourage people to adopt the technology (Nezamdoust et al. 2022).
Methodology
| Items | Perceived usefulness (Hu and O’Brien 2016) |
| 1 | Using information systems in the healthcare sector allows me to find the best deals. |
| 2 | The use of an information system enhances my effectiveness in the healthcare sector. |
| 3 | The use of information systems in the healthcare sector is useful to me. |
| 4 | The use of an information system saves time for me. |
| Perceived ease of use (Park 2009) | |
| 5 | Information system healthcare apps are easy to use. |
| 6 | The medical facility does not require much mental effort if supported by an information system (alternatives are offered by an information system). |
| 7 | Healthcare facilities are not so complicated if information systems offered services to me. |
| 8 | Learning to use an AI-powered healthcare information system is easy for me. |
| 9 | Becoming skillful at using healthcare information systems is easy. Financial strength/capability (Loke et al. 2015) |
| 10 | My organization responsibly used credit. |
| 11 | My organization can Invest money in a proper way. |
| 12 | My organization effectively budgets the money that they have. |
| 13 | My organization effectively spends its money on its daily needs. |
| 14 | My organization is fully capable of saving money. |
| Adoption of information system (Saeed and Abdinnour-Helm 2008) | |
| 15 | Information system pulls together services that are offered by different areas in the university. |
| 16 | Information systems effectively integrate services from different areas of the university. |
| 17 | The information system enables me to access services from anywhere within the university (dropped). |
| 18 | The information system provides data that is accurate. |
| 19 | The information system provides data that is well formatted. |
| 20 | The information system provides real-time data (dropped) information system provides real-time data (dropped). |
| 21 | Using the information system improves my effectiveness. |
| 22 | Using the Information system improves my performance. |
| 23 | Using the information system enhances my productivity. |
| 24 | Overall, using an information system is useful. |
| Number | Percentage | |
| Gender | ||
| Male | 317 | 52.7% |
| Female | 285 | 47.3% |
| Total | 602 | 100.0% |
| Age group | ||
| 20-30 years | 130 | 21.2% |
| 31-40 years | 268 | 43.7% |
| 41-50 years | 168 | 27.4% |
| 51 and above years | 36 | 5.9% |
| Total | 602 | 98.2% |
| Designation | ||
| Doctor | 315 | 52.3% |
| Nurse | 287 | 47.7% |
| Total | 602 | 100.0% |
the table indicates their age-wise distribution, which indicates that 130 were in the age group of
Results and findings
| Table 3 Reliability, multicollinearity, and convergent validity. | ||||||
| Construct | Items | Outer loadings | VIF | CA | CR | AVE |
| Adaptation of information system | AIS2 | 0.673 | 1.740 | 0.874 | 0.900 | 0.532 |
| AIS3 | 0.644 | 1.505 | ||||
| AIS4 | 0.735 | 1.993 | ||||
| AIS5 | 0.774 | 2.063 | ||||
| AIS6 | 0.713 | 1.895 | ||||
| AIS7 | 0.779 | 2.012 | ||||
| AIS8 | 0.703 | 1.748 | ||||
| AIS10 | 0.801 | 1.977 | ||||
| Financial capability | FSC1 | 0.747 | 1.885 | 0.883 | 0.914 | 0.680 |
| FSC2 | 0.848 | 2.214 | ||||
| FSC3 | 0.834 | 2.523 | ||||
| FSC4 | 0.886 | 2.921 | ||||
| FSC7 | 0.800 | 1.787 | ||||
| Perceived ease of use | PEU2 | 0.697 | 1.445 | 0.649 | 0.794 | 0.565 |
| PEU3 | 0.712 | 1.345 | ||||
| PEU4 | 0.838 | 1.175 | ||||
| Perceived usefulness | PUF1 | 0.805 | 2.295 | 0.882 | 0.907 | 0.583 |
| PUF2 | 0.781 | 2.206 | ||||
| PUF3 | 0.793 | 2.332 | ||||
| PUF4 | 0.699 | 1.885 | ||||
| PUF6 | 0.772 | 2.249 | ||||
| PUF7 | 0.734 | 1.704 | ||||
| PUF8 | 0.758 | 1.978 | ||||
| Size of hospital | SOH1 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Adaptation of information system | Financial capability | Perceived ease of use | Perceived usefulness | Size of hospital | |
| Adaptation of information system | 0.729 | ||||
| Financial capability | 0.274 | 0.825 | |||
| Perceived ease of use | 0.167 | 0.303 | 0.751 | ||
| Perceived usefulness | 0.315 | 0.737 | 0.312 | 0.764 | |
| Size of hospital | -0.015 | 0.121 | 0.09 | 0.143 | 1.000 |
| Adaptation of information system | Financial capability | Perceived ease of use | Perceived usefulness | |
| Financial capability | 0.292 | |||
| Perceived ease of use | 0.215 | 0.366 | ||
| Perceived usefulness | 0.34 | 0.837 | 0.389 | |
| Size of hospital | 0.065 | 0.131 | 0.095 | 0.16 |
| Hypothesis |
|
T Statistics |
|
Results |
| H1: FC -> AIS | 0.168 | 1.995 | 0.023 | Supported |
| H2: PEU -> AIS | 0.076 | 1.981 | 0.044 | Supported |
| H3: PU -> AIS | 0.254 | 4.162 | 0.000 | Supported |
| H4: FC/SOH/AIS > AIS | -0.075 | 1.246 | 0.213 | Not supported |
| H5: PEU/SOH/AIS > AIS | 0.101 | 2.618 | 0.009 | Supported |
| H6: PUS/SOH/AIS > AIS | 0.08 | 1.073 | 0.283 | Not supported |
The values of regression analysis show that there is positive and significant relationship between FC and the adoption of HIS with a
The values of regression analysis show that there is positive and significant relationship between PEU and the adoption of HIS with a
significant role of PEU in the adoption of HIS is positive and significant. In other words, PEU positively influence the adoption of HIS.
The values of regression analysis show that there is positive and significant relationship between PU and the adoption of HIS with a
| Saturated model | Estimated model | |
| SRMR | 0.068 | 0.068 |
| d_ULS | 1.391 | 1.391 |
| d_G | 0.524 | 0.524 |
| Chi-square | 1796.522 | 1796.522 |
| NFI | 0.76 | 0.76 |
| SSO | SSE |
|
|
Sig. R square | |
| AIS | 4816 | 4563.673 | 0.052 | 0.126 | 0.000 |
| FC | 3010 | 3010 | |||
| PEU | 1806 | 1806 | |||
| PU | 4214 | 4214 | |||
| SOH | 602 | 602 |
| Adaptation of information system | Importance | Performances |
| Financial capability | 0.078 | 62.56 |
| PEU | 0.101 | 59.022 |
| PU | 0.365 | 68.297 |
| Relationships |
|
|
| H1: FC -> AIS | -0.027 | 0.827 |
| H2: PEU -> AIS | 0.031 | 0.683 |
| H3: PU -> AIS | -0.157 | 0.190 |
| H4: FC/SOH/AIS -> AIS | 0.095 | 0.464 |
| H5: PEU/SOH/AIS -> AIS | -0.006 | 0.940 |
| H6: PUS/SOH/AIS -> AIS | 0.073 | 0.610 |
| Relationships |
|
|
| H1: FC -> AIS | 0.120 | 0.312 |
| H2: PEU -> AIS | 0.006 | 0.899 |
| H3: PU -> AIS | -0.270 | 0.027 |
| H4: FC/SOH/AIS -> AIS | 0.006 | 0.981 |
| H5: PEU/SOH/AIS -> AIS | 0.014 | 0.854 |
| H6: PUS/SOH/AIS -> AIS | -0.041 | 0.772 |
responsible for the adaptation of the IS (Chen et al. 2020). Six hypotheses were claimed based on this study’s model, among which three are based on direct relationships, and the other is based on moderating relationships. Among these six, only two hypotheses were not supported by the findings of this study, while the other four were supported. The first hypothesis claims that financial capability will lead to a better adaptation of the IS in the healthcare sector of Pakistan. However, the findings of this study support the claimed hypothesis with the
sensitive nature of data, which need the adoption of useful and user-friendly technologies (Huarng et al. 2022). Similarly, financial capability (Endriyas et al. 2023) of a healthcare organization is also critical as the adoption of HIS requires large investments in technological facilities, training, and maintenance. Hospitals might face difficulties in the adoption and integration of HIS if they have financial difficulties. This could impede their capacity to fully utilize HIS for better services. Therefore, consideration of PEU, PU and financial capability are essential determinants for HIS adopting strategies. In addition, the research also investigated the moderating influence of hospital size (Kraus et al. 2021) on the impact of PU, PEU and financial capability on the adoption of HIS. It is clear from the findings that hospital size has a moderating role on the impact of PEU on HIS adoption. In other words, the role of PEU on HIS adoption is dependent on the hospital size. PEU may impact the adoption of HIS in large hospitals more than in smaller hospitals, as large hospitals have more organizational resources and complexities than the smaller ones. Due to the importance of this moderating effect, PEU-enhancing measures must to be adapted according to the specific needs associated with hospital sizes. It is essential to understand the relationship between hospital size and PEU in influencing the adoption of HIS in order to establish tailored strategies and measures according to the various needs and difficulties, faced by different size healthcare organizations. As shown by the findings, there exists no significant moderating role of the hospital size on the relationship between financial capability, PU and the adoption of HIS. The influence of financial capability and PU on HIS adoption is similar in hospitals of various sizes. In other words, PU and funding capacity have a considerable impact on the decision to adopt HIS, regardless of the hospital’s size. The absence of this moderating impact suggests that tactics to increase PU and provide funding for the adoption of HIS should be widely used in all hospital of all size. It emphasizes the significance of these elements as broadly applicable drivers for the HIS adoption across all hospitals. The research has the following implications.
Conclusion
Recommendations.
- Health organizations should allocate funds to new technology adoption (Poon et al. 2004).
- For successful implementation or adoption of an IS, the firms should select the system that is perceived to be useful and effortless (Nezamdoust et al. 2022; Zaman et al. 2022).
- Hospitals, etc., should train their employees on the usefulness of the new system before implementation (Pedota et al. 2023).
- Large hospitals need more careful selection of HIS as many parties will be involved in the using (Yusif et al. 2022).
Limitations and future work.
- Other theories and variables can be incorporated into the framework in future to make it more comprehensive.
- Given that this study was taken in Pakistan, the framework could also be tested in other countries to test is generalizability.
- Further research is needed to explore the influence of hospital size on the relationship of PU and financial strength.
Data availability
Published online: 15 April 2024
References
Ahmad SF, Alam MM, Rahmat MK, Mubarik MS, Hyder SI (2022) Academic and administrative role of artificial intelligence in education. Sustainability 14(3):1101. https://doi.org/10.3390/su14031101
Ahmad SF, Rahmat MK, Mubarik MS, Alam MM, Hyder SI (2021) Artificial intelligence and its role in education. Sustainability 13(22):12902. https://doi. org/10.3390/su132212902
Akther T, Nur T (2022) A model of factors influencing COVID-19 vaccine acceptance: a synthesis of the theory of reasoned action, conspiracy theory belief, awareness, perceived usefulness, and perceived ease of use. PLoS ONE 17(1):e0261869. https://doi.org/10.1371/journal.pone. 0261869
Alboliteeh M, Alrashidi MS, Alrashedi N, Gonzales A, Mostoles RJ, Pasay-an E, Dator WL (2022) Knowledge management and sustainability performance of hospital organisations: the healthcare managers’ perspective. Sustainability 15(1):203. https://doi.org/10.3390/su15010203
Almaiah MA, Alhumaid K, Aldhuhoori A, Alnazzawi N, Aburayya A, Alfaisal R, Salloum SA, Lutfi A, Al Mulhem A, Alkhdour T, Awad AB, Shehab R (2022) Factors affecting the adoption of digital information technologies in higher education: an empirical study. Electronics 11(21):3572. https://doi.org/10. 3390/electronics11213572
Alotaibi Y, Subahi AF (2022) New goal-oriented requirements extraction framework for e-health services: a case study of diagnostic testing during the COVID-19 outbreak. Bus Process Manag J 28(1):273-292. https://doi.org/10. 1108/BPMJ-09-2020-0414
Alsyouf A, Lutfi A, Alsubahi N, Alhazmi FN, Al-Mugheed K, Anshasi RJ, Alharbi NI, Albugami M (2023) The use of a technology acceptance model (TAM) to predict patients’ usage of a personal health record system: the role of security, privacy, and usability. Int J Environ Res Public Health 20(2):1347. https://doi. org/10.3390/ijerph20021347
Barney J (1991) Firm resources and sustained competitive advantage. J Manag 17(1):99-120. https://doi.org/10.1177/014920639101700108
Bloomberg J (2018) Digitization, digitalization, and digital transformation: confuse them at your peril. Forbes
Broccardo L, Zicari A, Jabeen F, Bhatti ZA (2023) How digitalization supports a sustainable business model: a literature review. Technol Forecast Soc Change 187:122146. https://doi.org/10.1016/j.techfore.2022.122146
Brown SA, Dennis AR, Venkatesh V (2010) Predicting collaboration technology use: integrating technology adoption and collaboration research. J Manag Inf Syst 27(2):9-54. https://doi.org/10.2753/MIS0742-1222270201
Chen L, Aklikokou AK (2020) Determinants of E-government adoption: testing the mediating effects of perceived usefulness and perceived ease of use. Int J Public Adm 43(10):850-865. https://doi.org/10.1080/01900692.2019.1660989
Chen P-T, Lin C-L, Wu W-N (2020) Big data management in healthcare: adoption challenges and implications. Int J Inf Manag 53:102078. https://doi.org/10. 1016/j.ijinfomgt.2020.102078
Cheng N, Li H, Bang Y (2023) Pay-for-performance schemes and hospital HIT adoption. Decis Support Syst 164:113868. https://doi.org/10.1016/j.dss.2022. 113868
Crisan EL, Mihaila A (2023) Health-care information systems adoption-a review of management practices. Vilakshan XIMB J Manag 20(1):130-139. https:// doi.org/10.1108/XJM-04-2021-0121
Dewar RD, Dutton JE (1986) The adoption of radical and incremental innovations: an empirical analysis. Manag Sci 32(11):1422-1433
Davis FD (1989) Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q 13(3):319. https://doi.org/10.2307/249008
Deepu TS, Ravi V (2021) Supply chain digitalization: an integrated MCDM approach for inter-organizational information systems selection in an electronic supply chain. Int J Inf Manag Data Insights 1(2):100038. https://doi. org/10.1016/j.jjimei.2021.100038
Dhagarra D, Goswami M, Kumar G (2020) Impact of trust and privacy concerns on technology acceptance in healthcare: an Indian perspective. Int J Med Inform 141:104164. https://doi.org/10.1016/j.ijmedinf.2020.104164
Dicuonzo G, Donofrio F, Fusco A, Shini M (2023) Healthcare system: moving forward with artificial intelligence. Technovation 120:102510. https://doi.org/ 10.1016/j.technovation.2022.102510
Hedayati MK, Schniederjans DG (2022) Integration of knowledge management in digital healthcare industries. In: Wang J (ed) Encyclopedia of data science and machine learning. IGI Global United States of America, p 1703-1716. https:// doi.org/10.4018/978-1-7998-9220-5.ch102
Hopper AM (2015) Using data management techniques to modernize healthcare. Productivity Press
Huarng K-H, Yu TH-K, Lee CF (2022) Adoption model of healthcare wearable devices. Technol Forecast Soc Change 174:121286. https://doi.org/10.1016/j. techfore.2021.121286
Ibrahim M, Shahid MK, Ahmed SF (2014) The impact of telecom services characteristics on consumer for use in Pakistan. Adv Econ Bus 2(4):172-179. https://doi.org/10.13189/aeb.2014.020403
Ibrahim M, Shahid M, Akbar S, Ahmed SF (2015) Determining the effect of innovations for mobile banking adoption in Pakistan. J Inf Eng Appl 5(11):16-23
Jarva E, Oikarinen A, Andersson J, Tomietto M, Kääriäinen M, Mikkonen K (2023) Healthcare professionals’ digital health competence and its core factors; development and psychometric testing of two instruments. Int J Med Inform 171:104995. https://doi.org/10.1016/j.ijmedinf.2023.104995
Khan Y, Su’ud MBM, Alam MM, Ahmad SF, Ahmad (Ayassrah) AYAB, Khan N (2022a) Application of internet of things (IoT) in sustainable supply chain management. Sustainability 15(1):694. https://doi.org/10.3390/su15010694
Khan Y, Su’ud MBM, Alam MM, Ahmad SF, Salim NA, Khan N (2022b) Architectural threats to security and privacy: a challenge for internet of things (IoT) applications. Electronics 12(1):88. https://doi.org/10.3390/electronics12010088
Khanna RR, Murray SG, Wen T, Salmeen K, Illangasekare T, Benfield N, AdlerMilstein J, Savage L (2022) Protecting reproductive health information in the post-Roe era: interoperability strategies for healthcare institutions. J Am Med Inform Assoc 30(1):161-166. https://doi.org/10.1093/jamia/ocac194
Kim D-Y, Jang S (Shawn), Morrison AM (2011) Factors affecting organizational information technology acceptance: a comparison of convention and visitor bureaus and meeting planners in the United States. J Conv Event Touri 12(1):1-24. https://doi.org/10.1080/15470148.2010.551291
Kraus S, Schiavone F, Pluzhnikova A, Invernizzi AC (2021) Digital transformation in healthcare: analyzing the current state-of-research. J Bus Res 123:557-567. https://doi.org/10.1016/j.jbusres.2020.10.030
Kuan KKY, Chau PYK (2001) A perception-based model for EDI adoption in small businesses using a technology-organization-environment framework. Inf Manag 38(8):507-521. https://doi.org/10.1016/S0378-7206(01)00073-8
Kuek A, Hakkennes S (2020) Healthcare staff digital literacy levels and their attitudes towards information systems. Health Inform J 26(1):592-612. https:// doi.org/10.1177/1460458219839613
LaBerge L (2020) How COVID-19 has pushed companies over the technology tipping point-and transformed business forever. Mckinsey. https://www. mckinsey.com/capabilities/strategy-and-corporate-finance/our-insights/how-covid-19-has-pushed-companies-over-the-technology-tipping-point-and-transformed-business-forever
Lee G, Xia W (2006) Organizational size and IT innovation adoption: a metaanalysis. Inf Manag 43(8):975-985. https://doi.org/10.1016/j.im.2006.09.003
Lin C, Lin I-C, Roan J (2012) Barriers to physicians’ adoption of healthcare information technology: an empirical study on multiple hospitals. J Med Syst 36(3):1965-1977. https://doi.org/10.1007/s10916-011-9656-7
Liu X, Ahmad SF, Anser MK, Ke J, Irshad M, Ul-Haq J, Abbas S (2022) Cyber security threats: a never-ending challenge for e-commerce. Front Psychol 13. https://doi.org/10.3389/fpsyg.2022.927398
Lind MR, Zmud RW, Fischer WA (1989) Microcomputer adoption-the impact of organizational size and structure. Inf Manag 16(3):157-162
Loke V, Choi L, Libby M (2015) Increasing Youth Financial Capability: An Evaluation of the MyPath Savings Initiative. J Consum Aff 49(1):97-126. https:// doi.org/10.1111/joca. 12066
Mahdi SS, Battineni G, Khawaja M, Allana R, Siddiqui MK, Agha D (2023) How does artificial intelligence impact digital healthcare initiatives? A review of AI applications in dental healthcare. Int J Inf Manag Data Insights 3(1):100144. https://doi.org/10.1016/j.jjimei.2022.100144
Malik M, Kazi AF, Hussain A (2021) Adoption of health technologies for effective health information system: need of the hour for Pakistan. PLoS ONE 16(10):e0258081. https://doi.org/10.1371/journal.pone. 0258081
McAdory BJ (2021) Investment in information technology can improve profitability in U.S. hospitals. https://harbert.auburn.edu/news/investment-in-information-technology-can-improve-profitability-in-us-hospitals.html
Mousa S, Bouraoui T (2023) The role of sustainability and innovation in financial services business transformation. Theor Econ Lett 13(1):84-108. https://doi. org/10.4236/tel.2023.131005
Ndayishimiye C, Lopes H, Middleton J (2023) A systematic scoping review of digital health technologies during COVID-19: a new normal in primary health care delivery. Health Technol. https://doi.org/10.1007/s12553-023-00725-7
Nezamdoust S, Abdekhoda M, Rahmani A (2022) Determinant factors in adopting mobile health application in healthcare by nurses. BMC Med Inform Decis Mak 22(1):47. https://doi.org/10.1186/s12911-022-01784-y
Nikou S, Maslov I (2021) An analysis of students’ perspectives on e-learning participation-the case of COVID-19 pandemic. Int J Inf Learn Technol 38(3):299-315. https://doi.org/10.1108/IJILT-12-2020-0220
Park DY, Kim H (2023) Determinants of intentions to use digital mental healthcare content among university students, faculty, and staff: motivation, perceived usefulness, perceived ease of use, and parasocial interaction with AI Chatbot. Sustainability 15(1):872. https://doi.org/10.3390/su15010872
Park SY (2009) An Analysis of the Technology Acceptance Model in Understanding University Students’ Behavioral Intention to Use e-Learning. Edu Technol Soc 12(3):150-162
Pedota M, Grilli L, Piscitello L (2023) Technology adoption and upskilling in the wake of Industry 4.0. Technol Forecast Soc Change 187:122085. https://doi. org/10.1016/j.techfore.2022.122085
Philibert C (2003) Technology innovation, development and diffusion. https:// www.oecd.org/env/cc/2956490.pdf
Poon EG, Blumenthal D, Jaggi T, Honour MM, Bates DW, Kaushal R (2004) Overcoming barriers to adopting and implementing computerized physician order entry systems in U.S. hospitals. Health Aff 23(4):184-190. https://doi. org/10.1377/hlthaff.23.4.184
Prasad A (2018) 10 ways technology has reshaped the modern workplace. Quickfms. https://www.quickfms.com/blog/how-technology-has-reshaped-the-workplace
Pufahl L, Zerbato F, Weber B, Weber I (2022) BPMN in healthcare: challenges and best practices. Inf Syst 107:102013. https://doi.org/10.1016/j.is.2022.102013
Renny, Guritno S, Siringoringo H (2013) Perceived usefulness, ease of use, and attitude towards online shopping usefulness towards online airlines ticket purchase. Procedia Soc Behav Sci 81:212-216. https://doi.org/10.1016/j. sbspro.2013.06.415
Rey-Moreno M, Periáñez-Cristóbal R, Calvo-Mora A (2022) Reflections on sustainable urban mobility, mobility as a service (MaaS) and adoption models. Int J Environ Res Public Health 20(1):274. https://doi.org/10.3390/ ijerph20010274
Rohani N, Yusof MM (2023) Unintended consequences of pharmacy information systems: a case study. Int J Med Inform 170:104958. https://doi.org/10.1016/j. ijmedinf.2022.104958
Saeed KA, Abdinnour-Helm S (2008) Examining the effects of information system characteristics and perceived usefulness on post adoption usage of information systems. Inf Manag 45(6):376-386. https://doi.org/10.1016/j. im.2008.06.002
Salah OH, Yusof ZM, Mohamed H (2021) The determinant factors for the adoption of CRM in the Palestinian SMEs: the moderating effect of firm size. PLoS ONE 16(3):e0243355. https://doi.org/10.1371/journal.pone. 0243355
Sayed AF, Shahid MK, Ahmad SF (2020) Adoption of mobile payment application and its impact on business. pp. 253-269. https://doi.org/10.4018/978-1-7998-2398-8.ch012
Shahadat MMH, Nekmahmud M, Ebrahimi P, Fekete-Farkas M (2023) Digital technology adoption in SMEs: what technological, environmental and organizational factors influence in emerging countries? Glob Bus Rev 097215092211371. https://doi.org/10.1177/09721509221137199
Shahzad K, Jianqiu Z, Zia MA, Shaheen A, Sardar T (2021) Essential factors for adopting hospital information system: a case study from Pakistan. Int J Comput Appl 43(1):26-37. https://doi.org/10.1080/1206212X.2018.1504460
Singerman A, Lence SH (2023) The source of uncertainty influences technology adoption. Eur Rev Agric Econ. https://doi.org/10.1093/erae/jbac036
Sinhasane S (2022) What is health information system and its significance in the healthcare sector? https://mobisoftinfotech.com/resources/blog/importance-of-health-information-system/
Stachwitz P, Debatin JF (2023) Digitalisierung im Gesundheitswesen: heute und in Zukunft. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 66(2):105-113. https://doi.org/10.1007/s00103-022-03642-8
Sturmberg JP, Bircher J (2019) Better and fulfilling healthcare at lower costs: the need to manage health systems as complex adaptive systems. F1000Research 8:789. https://doi.org/10.12688/f1000research.19414.1
Tortorella GL, Fogliatto FS, Espôsto KF, Mac Cawley Vergara A, Vassolo R, Tlapa Mendoza D, Narayanamurthy G (2022) Measuring the effect of Healthcare 4.0 implementation on hospitals’ performance. Prod Plan Control 33(4):386-401. https://doi.org/10.1080/09537287.2020.1824283
Tsai M-F, Hung S-Y, Yu W-J, Chen CC, Yen DC (2019) Understanding physicians’ adoption of electronic medical records: healthcare technology self-efficacy, service level and risk perspectives. Comput Stand Interfaces 66:103342. https://doi.org/10.1016/j.csi.2019.04.001
Tseng M-L, Ha HM, Wu K-J, Xue B (2022) Healthcare industry circular supply chain collaboration in Vietnam: vision and learning influences on connection in a circular supply chain and circularity business model. Int J Logist Res Appl 25(4-5):743-768. https://doi.org/10.1080/13675567.2021.1923671
Vassolo RS, Mac Cawley AF, Tortorella GL, Fogliatto FS, Tlapa D, Narayanamurthy G (2021) Hospital investment decisions in healthcare 4.0 technologies: scoping review and framework for exploring challenges, trends, and research directions. J Med Internet Res 23(8):e27571. https://doi.org/10. 2196/27571
Veikkolainen P, Tuovinen T, Jarva E, Tuomikoski A-M, Männistö M, Pääkkönen J, Pihlajasalo T, Reponen J (2023) eHealth competence building for future doctors and nurses-attitudes and capabilities. Int J Med Inform 169:104912. https://doi.org/10.1016/j.ijmedinf.2022.104912
Venkatesh V, Thong JYL, Xu X (2012) Consumer acceptance and use of information technology: extending the unified theory of acceptance and use of technology. MIS Q 36(1):157. https://doi.org/10.2307/41410412
Wang BB, Wan TTH, Burke DE, Bazzoli GJ, Lin BYJ (2005) Factors influencing health information system adoption in American hospitals. Health Care Manag Rev 30(1):44-51
Xiong E (2021) The sustainable impact of a paperless office. Forbes. https://www. forbes.com/sites/forbestechcouncil/2021/05/11/the-sustainable-impact-of-a-paperless-office/?sh=1fb81b421095
Yulianto A, Ahmad S, Lelly A, Nobia S (2022) Ease of use technology as a dominant factor in technology acceptance hospital information system by officers at the Jambi provincial government hospital. In: Proceedings of the 5th European international conference on industrial engineering and operations management Rome, Italy, July 26-28, 2022. IEOM Society International
Yusif S, Hafeez-Baig A, Soar J (2022) Change management and adoption of health information technology (HIT)/eHealth in public hospitals in Ghana: a qualitative study. Appl Comput Inform 18(3/4):279-289. https://doi.org/10.1016/ j.aci.2019.11.007
Zhao Y, Li K, Zhang L (2019) A meta-analysis of online health adoption and the moderating effect of economic development level. Int J Med Inform 127:68-79. https://doi.org/10.1016/j.ijmedinf.2019.04.015
Acknowledgements
Author contributions
Competing interests
Ethical approval
Informed consent
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
© The Author(s) 2024
The School of Economics and Management, Shanghai Polytechnic University, Shanghai 201209, China. Institute of Business Management, Karachi, Pakistan. College of Business Administration, King Saud University, Riyadh, Saudi Arabia. International Institute of Social Studies (ISS), Erasmus University Rotterdam, Kortenaerkade 12, 2518 AX The Hague, The Netherlands. Department of Management Sciences, University of Gwadar, Gwadar, Pakistan. email: fayaz.ahmed@iobm.edu.pk; ou@iss.nl
